Heart-wrenching
Father’s health scare leads to reflections on life and the realities of aging
Advertisement
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.95 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.99/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19.95 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 16/12/2024 (391 days ago), so information in it may no longer be current.
Last month, I came close to losing my dad.
It was a typical Thursday afternoon when my sister, Luisa, and I got a text from our mom, Gina. She said she had called emergency services because our dad was struggling to breathe and paramedics had rushed him to Grace Hospital.
The next few moments felt like a blur. I knew my 75-year-old dad, Pasquale, had been dealing with a lingering cough and was prone to bronchitis — was that what this was or was it something more serious?

When I arrived at the Grace’s emergency department, a nurse informed me they had managed to stabilize my dad but that he had been dangerously close to cardiac arrest upon arrival.
Wait, what? When did that happen — and how?
They pulled back the curtain and there was my dad. He was wearing a CPAP machine and was connected to several other devices. A CPAP (continuous positive airway pressure) machine helps push oxygen into the lungs through a mask covering the nose or mouth. It’s commonly used for people with sleep apnea.
While my dad was breathing, he needed the machine’s support to do so effectively. He looked pale and in shock, understandably. I had arrived just before my mom and sister, so I did my best to reassure him, explain where he was, what had happened and that he was in good hands.
The emergency doctor explained that my dad had experienced respiratory failure and had been only 15 to 30 minutes away from cardiac arrest. When he arrived at the hospital, his blood pressure was dangerously high and they had to act quickly to bring it down. Had he suffered a heart attack, his outcome would have been drastically different. We’re grateful that my mom called 911 when she did.
The fear of watching your parents age is incredibly real. Going from thinking, “My dad is the strongest person I know,” to seeing him struggle to breathe was a harsh reality. It was a wake-up call I didn’t want but couldn’t avoid. As I grow older, so do my parents — day by day, they’re aging and falling ill more frequently.
The hardest part? There’s nothing I can do to stop it. All I can do is feel a piece of myself break down if my mom has a joint ache or, in this case, see my dad lying in a hospital bed. I don’t even really think of my dad as old — and I’m not just saying that to flatter him, should he read this some day.
We often hear about the shortcomings and challenges in our health-care system and many of those concerns are undoubtedly valid. Everyone’s experience is unique and we acknowledge that. But the reality is, those doctors saved my dad’s life. The care he received from the hospital team was exceptional and he understands just how fortunate he was.
We learned from the doctors that my dad had pneumonia — an incredibly dangerous condition for anyone, especially a 75-year-old — which had placed significant strain on my poor dad’s heart.
“Any acute medical condition causes strain on a person’s body. Pneumonia, for instance, can reduce oxygen levels, trigger inflammation and increase stress on the heart,” Dr. Anita Soni, medical lead of cardiac services at St. Boniface Hospital, told me.
After further testing, the doctors explained that my dad has aortic stenosis, a condition in which the valve between the heart and the aorta becomes narrowed, restricting blood flow and causing the heart to work harder. The strain from the pneumonia had constricted his heart valve even further to the point where medical intervention was necessary.
While we had known about his narrowed aortic valve — he had annual checkups with a cardiologist and it hadn’t caused issues until now — we didn’t know how dangerous pneumonia could be for someone with a heart-valve condition.
“The added stress that occurs with conditions such as pneumonia can cause the already overworked heart to decompensate further and lead to serious effects such as heart failure,” Soni says.
Aside from this incident, my dad is generally in good health. He’s mindful of his diet and takes medication for his blood pressure. I should mention, leading up to this event, my dad smoked for nearly 40 years (apart from the five years he quit in the 1980s). However, since this hospital stint, he’s been cigarette-free.
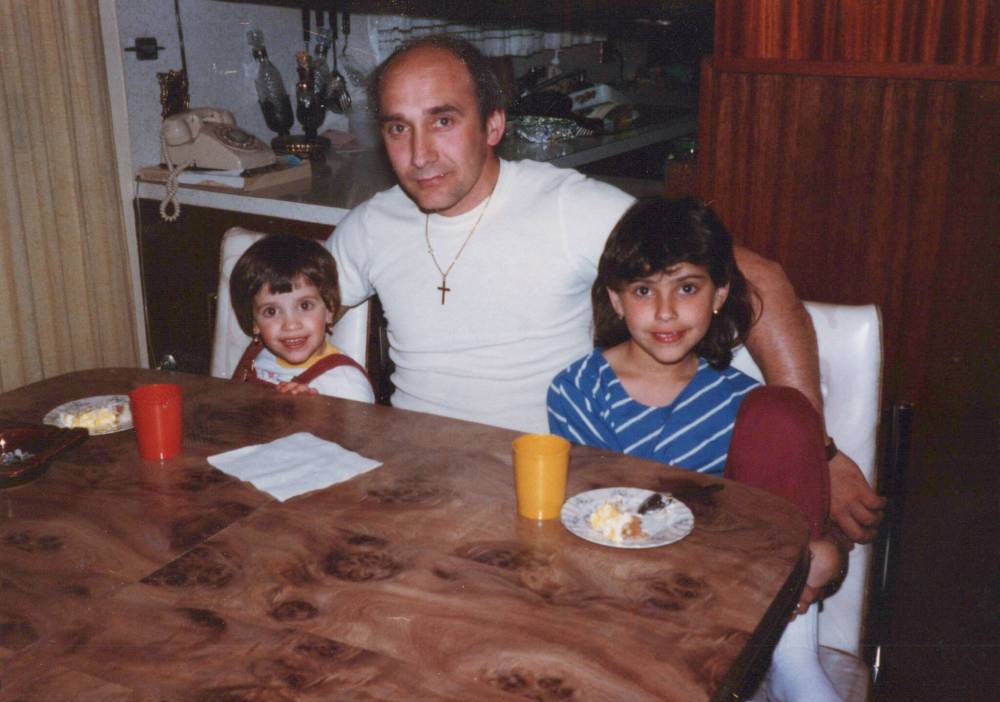
My dad leads an active life with a busy social calendar — he meets his friends for an espresso and a game of cards almost every day (Italians, right?), gets together with them on Friday nights and has been part of a bowling league with my mom on Tuesdays for the past four decades. My sister and I often joke that his social life is busier than ours.
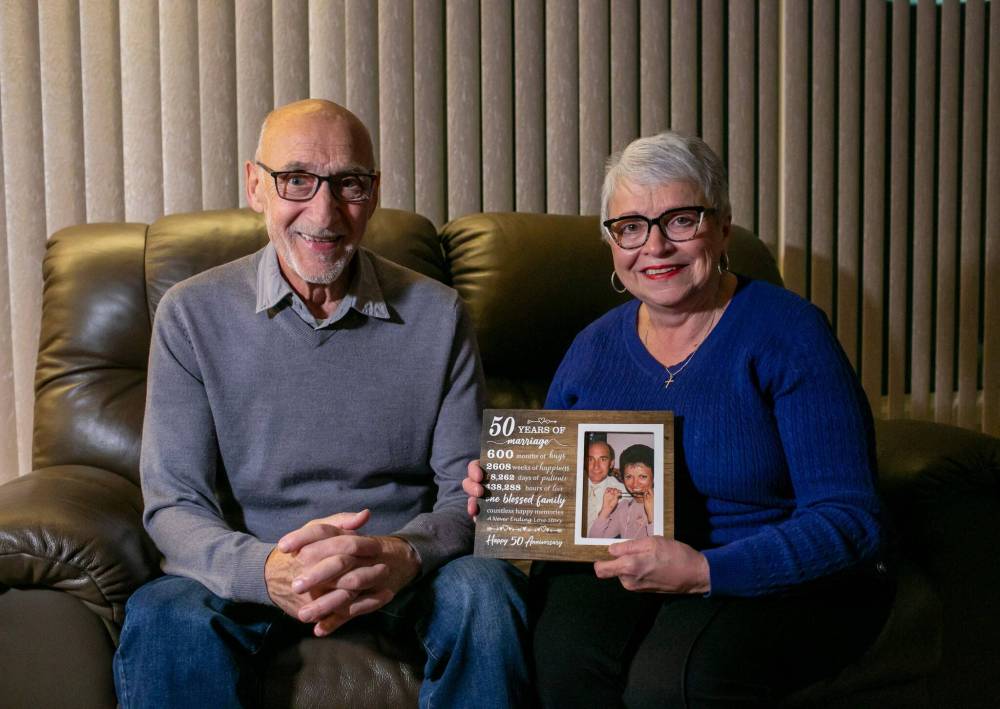
My parents also celebrated their 50th wedding anniversary two months ago with a group of family and friends.
I truly appreciate that my dad has meaningful social activities, especially at this stage of his life. Research shows they play a vital role in boosting mental health, enhancing life satisfaction and improving overall quality of life.
The doctors explained that my dad’s aortic stenosis would need to be addressed. However, given his age, open-heart surgery carried a higher risk. Instead, doctors performed various tests, including an echocardiogram (an ultrasound of the heart), a CT scan and an angiogram (to check for blocked arteries) to determine if he was a candidate for a TAVI (transcatheter aortic valve implantation) — a minimally invasive procedure that replaces a damaged aortic valve with a new one.
My dad was relieved when he learned he was eligible, sparing him from the challenges of major open-heart surgery.
“The first TAVI was done in an experimental fashion in the early 2000s. After many rounds of intensive scientific investigations, it was approved for commercial use in some fashion in most places around the world in the five to 10 years that followed,” says Dr. Aaron Spooner, a cardiac specialist at St. Boniface Hospital, adding that Winnipeg started its TAVI program a little over 10 years ago.
My dad underwent the TAVI procedure at St. B. During the procedure, a flexible, hollow tube called a catheter is guided through blood vessels, typically accessed via the groin, to reach the heart. The new valve is then delivered through the catheter, placed over the old one, and implanted securely.
Dr. Spooner says that elderly patients or those with additional medical conditions are often steered toward the TAVI, rather than open-heart surgery, due to its multiple advantages, including a quicker recovery time. However, he notes that because the procedure is relatively new, there isn’t yet enough long-term data on how well patients fare over time or how durable the valves ultimately are.
Manitoba performs about 200 TAVI procedures each year, which, per capita, is the lowest of any province, says a spokesperson from Doctors Manitoba.
“Manitoba should likely be doing somewhere around 350 to 400 TAVIs each year to keep up with the needs of our population. What’s needed is more resources, including nursing and other health-care workers. Looking more broadly at cardiac care, Manitoba also has a shortage of cardiac specialists, including cardiologists,” the spokesperson said.
My dad was discharged the day after his TAVI procedure. His vital signs and heart showed positive signs of recovery and he will now undergo several followup tests and appointments to ensure his new valve is functioning properly.
When the TAVI program was first introduced in Winnipeg in 2012, patients were put to sleep, similar to traditional surgery, and typically remained in the hospital for several days to a week following the procedure, Soni says.
“Now, patients are awake and talking through the procedure and typically stay in the hospital for a day or two afterward. Some patients even go home the same day,” she says.
What became a three-week hospital stay for my dad was, to say the least, a wake-up call. Life is unpredictable and you never know when it will throw you a curveball. Between my mom, sister and me, at least one of us was with my dad every day. My mom, ever the devoted caregiver, stayed by his side the entire time, even sleeping on a recliner in his hospital room for the first four nights. We got to know the hospital staff well and we even celebrated my birthday with them and the other patients in the family room.
My dad and I are very close and always have been. The thought of one day not having him in my life was overwhelming and I just wasn’t ready for that. There are more Winnipeg Jets games to watch together, local news stories to debate and anniversaries to celebrate.

The truth is, as a society, we’re getting older. According to the 2024 National Caregiving Survey from the Canadian Centre for Caregiving Excellence, the percentage of people aged 65 and older has been steadily increasing over the past 25 years. In 2022, they made up nearly 19 per cent of the total population. This number is projected to rise to 23 per cent by 2043.
I think the fear of loss, particularly when it comes to parents, is complex and deeply layered. It spans from thoughts such as “What will I do without them?” to “Why are my strong parents suddenly so vulnerable?” to “Who will love me the way they do?”
It also brings the reality of shifting from being cared for to becoming a caregiver yourself. It’s a delicate balance of trying to help them while still respecting their right to make their own choices. At least, that’s what I went through.
My dad is now recovering at home, taking it easy and cherishing simple joys, such as having dinner with my mom, sleeping in his own bed and spending the upcoming holidays with his family. And, of course, going for coffee with his friends.
To the doctors, nurses, paramedics and all staff at the Grace and St. B who cared for my dad, please know that you changed our lives by saving his.
sabrinacarnevale@gmail.com

Sabrina Carnevale is a freelance writer and communications specialist, and former reporter and broadcaster who is a health enthusiast. She writes a twice-monthly column focusing on wellness and fitness.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.

