HSC Canada’s worst-performing hospital, some Manitoba health care no better under NDP: nurses union report Grace, St. B, Brandon General among bottom eight facilities, according to national agency’s data
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.95 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.99/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19.95 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 12/02/2025 (330 days ago), so information in it may no longer be current.
Winnipeg’s Health Sciences Centre has earned the dismal distinction of being the worst-performing hospital in Canada.
The province’s largest hospital has the highest standardized mortality ratio in the country, according to data from the Canadian Institute for Health Information.
That, and more, was revealed Wednesday in a report released by the Manitoba Nurses Union that charged “no measurable progress has been observed” in some facets of health care since the New Democratic Party took power in the fall of 2023.
The 36-page report — dubbed the White Paper — takes aim at the provincial government, which took issue with the document and said it failed to account for ongoing system improvements or those already completed.
Union president Darlene Jackson stood by the report’s findings, saying the data contained within “cannot be disputed.
“I think this is a wake-up call for the public to say to government this is not acceptable,” Jackson told the Free Press. “Things are not rosy in health care, despite what’s been said. We are in a terrible crisis.”
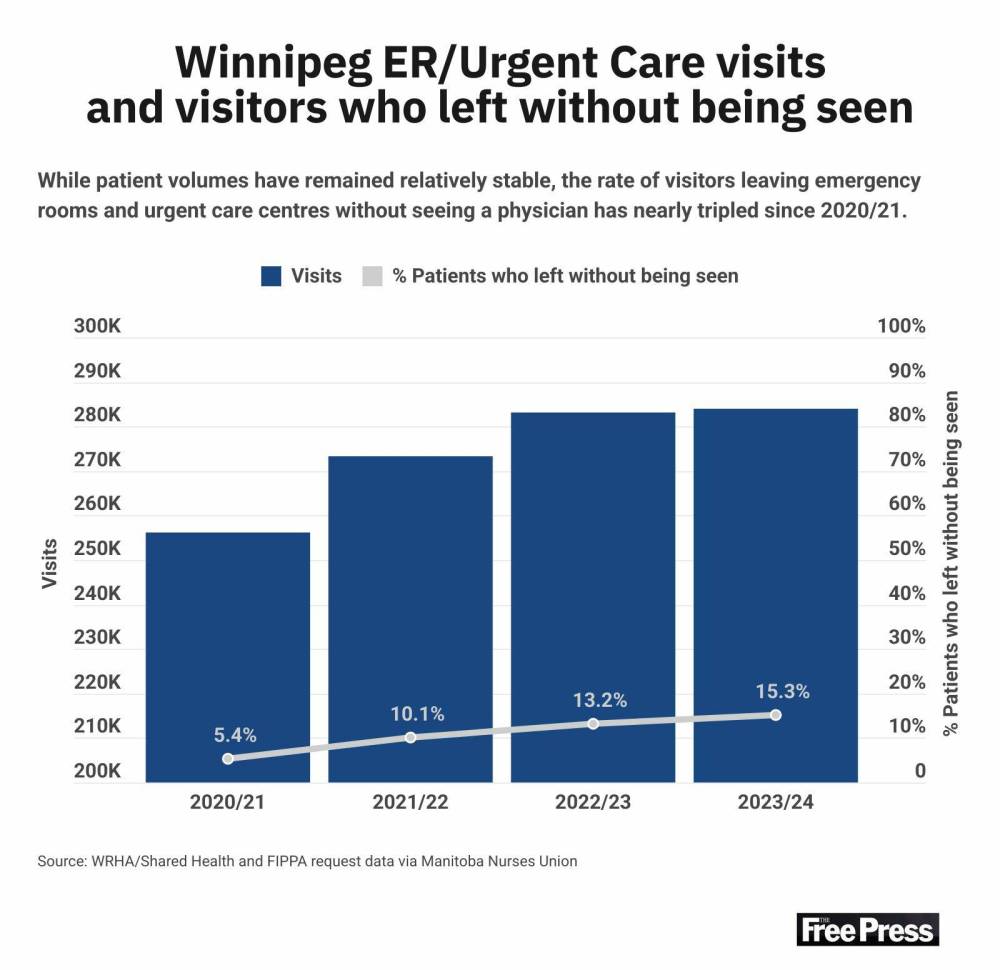
Using publicly available information and data obtained through freedom of information requests, the nursing union found the patient load of Winnipeg emergency departments and urgent-care centres has remained relatively consistent over the past five years.
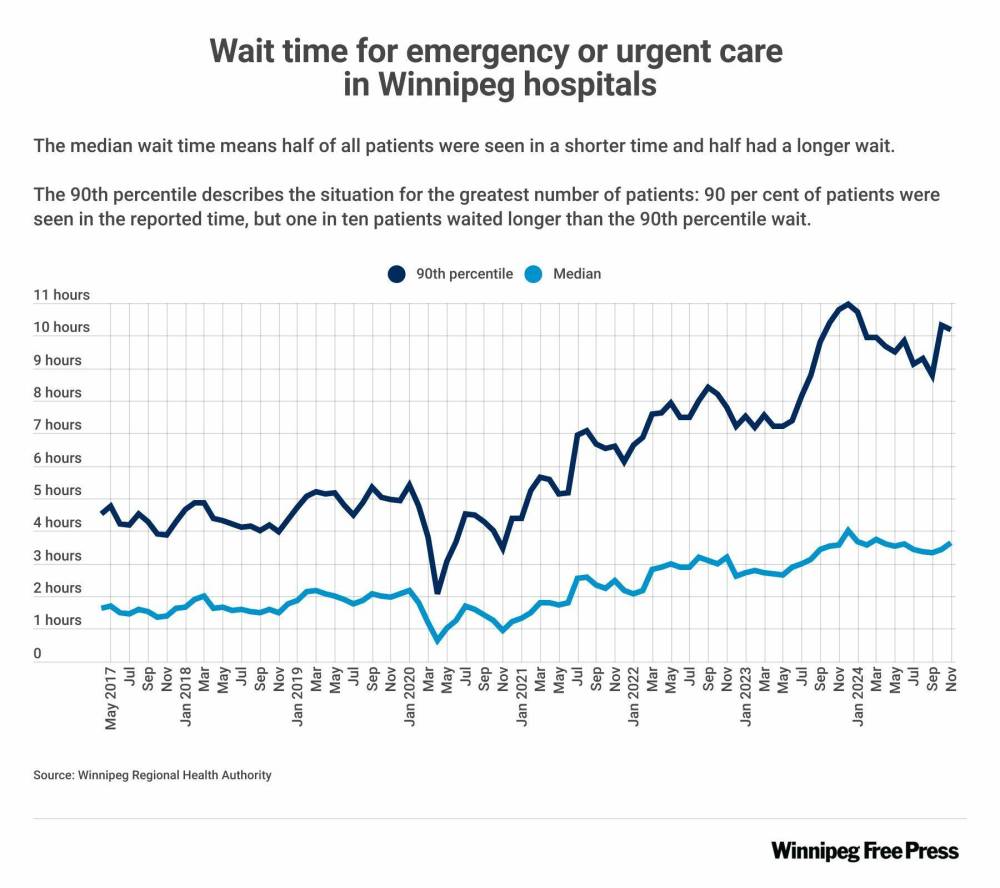
Wait times, however, have more than doubled, forcing one in seven patients to leave without receiving treatment, the report said.
“These statistics point to deep systemic issues that are compromising patient care and safety across Manitoba’s public health-care system,” it said.
CIHI’s standardized mortality ratio metric compares the mortality rates of hospitals nationwide, adjusting for factors such as age, sex, diagnoses, among others.
The institute’s most recent analysis, completed last year, found the Grace, St. Boniface and Brandon General hospitals also ranked among the eight worst-performing facilities in Canada.
“I feel terribly for the staff because I know how hard they work. I know that they are doing the best they can to provide amazing patient care, but circumstances have put them in this category, which is extremely sad,” Jackson said.
“Our nurses tell us continuously that things are not getting better in health care, that, in fact, there are areas where things are deteriorating. Nurses are frustrated. We were promised a change.”
In response, Shared Health issued a statement that said the hospital standardized mortality ratio “is not an accurate reflection of the highly skilled, patient-centred care a centre like HSC provides to a complex patient population.”
“As Manitoba’s trauma centre, Health Sciences Centre serves as the major referral centre for rural, northern and remote locations, and provides specialized care to the sickest and most severely injured patients from across our province. Those factors, combined with a population that has high rates of chronic disease, multiple co-morbidities and poor social determinants of health, make the interpretation of this data set challenging. Its validity has been called into question in the past for these reasons.”
Other data collected in the report showed nursing vacancy rates reached 21 per cent last summer, up from 16 per cent during the same period in 2020.
While the union admitted those numbers may have since improved, the report said the vacancies were “adversely affecting patient safety and the quality of care” as nursing overtime hours surged from 800,000 in 2021 to more than 1.1 million in 2024.
The province, in turn, spent $75 million on private-agency nurses to cover 1.2 million nursing hours last year, the report said, citing data it obtained from regional health authorities.
The government announced last week it added 1,255 net new hires in hospitals across Manitoba, including 481 nurses. Approximately 60 people came out of retirement and more than 200 left the private sector for the public system, Health Minister Uzoma Asagwara said.
“The concerns that are outlined in the White Paper are concerns that we have been taking very seriously, and we’ve taken action over these past 16 months to address,” Asagwara said.
“In some cases, the issues have actually already been completely addressed.”
Asagwara acknowledged there were challenges in health care, but said the government has made strides to bolster the system by listening to workers and investing in front-line care.
The minister pointed to safety improvements on the HSC campus as one recent example.
Asagwara has also directed health leaders to divert eight per cent of the dollars earmarked for corporate services to improve patient care before the end of the current fiscal year.
The union called the approach “short-sighted” and said it undermines new graduate support and senior nurse retention.
“(The) budget reduction ultimatum has effectively forced health authorities to cut costs rather than invest in proven retention strategies,” the report said.
The document included a slate of recommendations for the provincial government. Several were quality-of-life improvements, including creating a centralized shift scheduling system and providing better support for float nurses.
The province must also boost incentives to retain senior nurses, further improve facility safety measures, increase transparency by proactively releasing health-care metrics, invest in home-care nurses and address primary-care shortages by making better use of highly qualified nurse practitioners, the report said.
The union is hosting a news conference Thursday to further discuss the data it uncovered while preparing the report, Jackson said.
tyler.searle@freepress.mb.ca

Tyler Searle is a multimedia producer who writes for the Free Press’s city desk. A graduate of Red River College Polytechnic’s creative communications program, he wrote for the Stonewall Teulon Tribune, Selkirk Record and Express Weekly News before joining the paper in 2022. Read more about Tyler.
Every piece of reporting Tyler produces is reviewed by an editing team before it is posted online or published in print — part of the Free Press‘s tradition, since 1872, of producing reliable independent journalism. Read more about Free Press’s history and mandate, and learn how our newsroom operates.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.
History
Updated on Wednesday, February 12, 2025 6:42 PM CST: Adds statement from Shared Health.