Aides to check on patients waiting at HSC emergency in wake of death Report into death of 49-year-old in January lists 17 recommendations
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then price increases to the regular rate of $19.00 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.75/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 01/05/2025 (227 days ago), so information in it may no longer be current.
Manitoba’s emergency rooms will use more non-nursing staff to check on patients in waiting rooms after a man died in the Health Sciences Centre ER in January.
Chad Giffin, 49, had been waiting in the province’s busiest ER for about eight hours when staff noticed his condition had deteriorated. He was pronounced dead a short time later.
His death on Jan. 7 led to a critical incident review, which produced 17 recommendations aimed at preventing similar deaths in ERs across Manitoba.
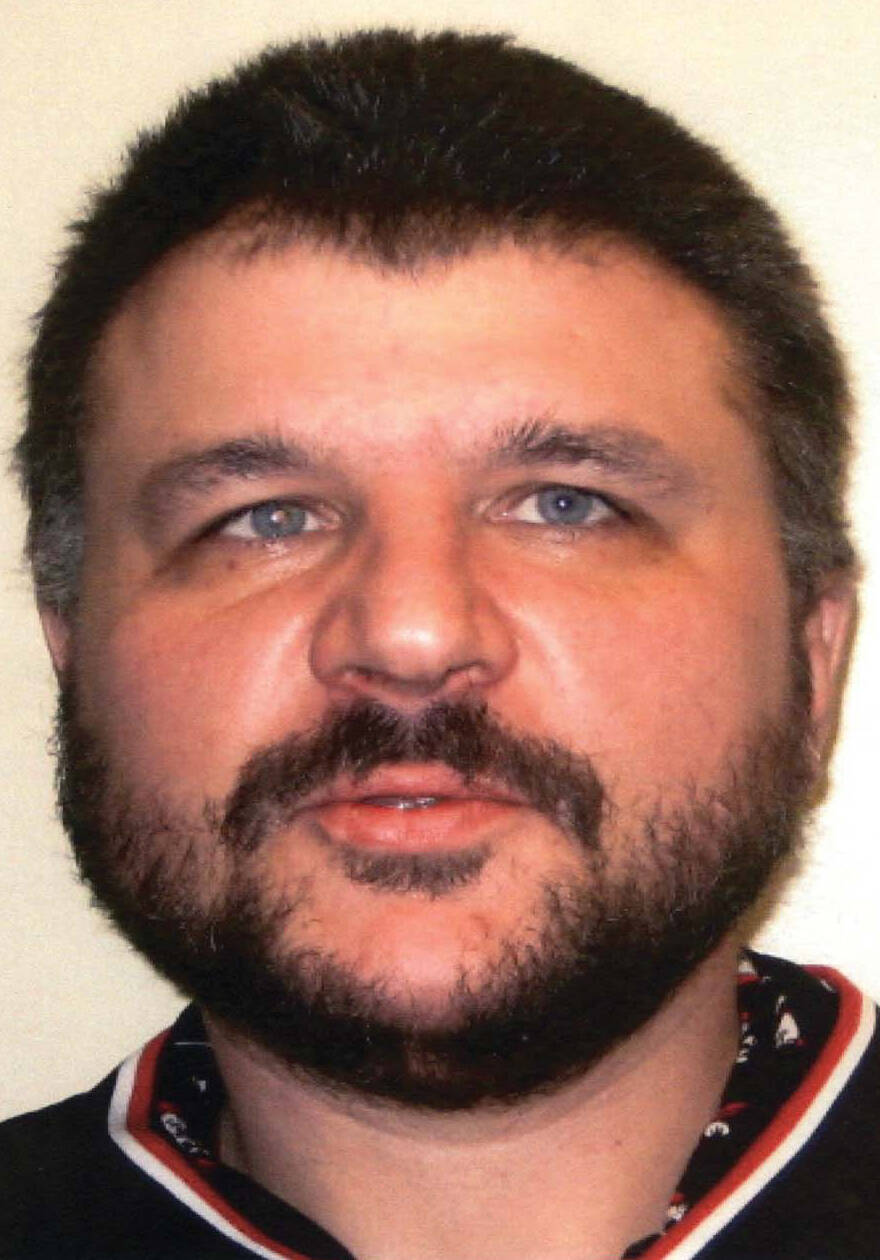
SUPPLIED
Chad Giffin died Jan. 7 in the ER waiting room at HSC. His death resulted in a review that produced 17 recommendations aimed at preventing similar deaths in ERs across Manitoba.
The recommendations
The Manitoba government said 17 recommendations were made during a critical incident review following the death of Chad Giffin in Health Sciences Centre’s emergency room in January.
The Manitoba government said 17 recommendations were made during a critical incident review following the death of Chad Giffin in Health Sciences Centre’s emergency room in January.
Action has been taken on all of them, Health Minister Uzoma Asagwara said.
- Training was implemented for 15 health-care aides to perform vitals checks on patients in the emergency department. One health-care aide position was dedicated to the task 24-7. A further 44 unit assistants were added to support the work.
- Staffing schedules were reviewed to ensure emergency departments were operating at baseline, and staff on shift were trained to use automated external defibrillators.
- An internal waiting room surge protocol was developed.
- Enhanced oversight and communication: reinforcing protocols with staff during daily huddles, reviewing 10 patient records a week for protocols, and reviewing community support worker logs to ensure hourly rounds are done on patients.
- Service delivery organizations were instructed to review and amend policies related to notifying next of kin in cases involving the death of a patient under the care of the public guardian and trustee. Policies should reflect that familial next of kin must be contacted.
- Larger system-wide improvements to improve wait times and patient flow (beyond HSC’s emergency department) are underway that look at improving staffing models, community care program enhancements and expanding care on weekends.
- Shared Health and the Winnipeg Fire Paramedic Service’s joint operation committee advocated for a review of transport destination algorithms with the intent to safely diversify receiving sites.
- Current guidelines to address the triage process were reviewed and updated to focus on the value of direct assessment.
- To develop a process to ensure staff assignments to the triage area are equitably distributed amongst all triage trained nurses.
- Assessing options to expand/enhance several lower-acuity patient units to reduce overcrowding.
- Reviewing supportive services that are part of capacity and flow protocols (like surge protocols) to expand or enhance night and weekends.
- Aligning, prioritizing, triaging and monitoring processes with practices in triage when the space is crowded with triaged patients waiting to be seen, patients awaiting followup, family and support people, members of the public.
- Exploring alternative points of entry through direct admission processes for transfers and specialist consultations.
- Reviewing staffing models in the waiting room and contingency planning during times of high patient volumes to support nursing reassessment.
- Environmental reviews of the waiting room to improve lines of site from triage and opportunities to enhance privacy during assessments.
- Installing weapon-detection technology in the emergency department and developing a harm-reduction strategy that addresses risks within the ED, as well as expanding supports for social workers in the ED.
- Reviewing internal communication and information systems to highlight care needs, clarify actions and roles.
“That particular situation, that tragedy, provided opportunities for us as a system to improve and to learn, and that work continues to be done,” Health Minister Uzoma Asagwara said at an unrelated event Thursday.
HSC officials had said Giffin was assessed, triaged as low acuity, or less urgent, and directed to the waiting room with instructions to speak to staff if his condition changed or worsened.
The over-capacity ER had about 100 patients, including 50 in the waiting room.
At the time, officials said the number of nurses on shift was just below the baseline. A government spokeswoman said Thursday staffing was later confirmed to be at the baseline. A backlog, or access block, prevented admitted ER patients from being moved to a bed elsewhere.
Among the 17 recommendations, the province said training was implemented for 15 health-care aides to conduct checks on patients in the hospital ER, along with one health-care aide position to provide 24-7 coverage. A further 44 unit assistants were added to support the work.
The purpose is to improve patient monitoring and ease pressure on nurses.
“What we’ve done, as a government, is make sure that consistently across our emergency departments not only are they staffing to baseline, but going above that by utilizing the skills of health-care aides who are trained and have the tools to do assessments like vital signs and other things that can help ensure people are getting care in the emergency department,” Asagwara said.
Margaret Schroeder, president of CUPE Local 204, which represents health-care aides at HSC, said additional community support workers were assigned to the HSC emergency department after the death of Brian Sinclair in 2008.
Schroeder said she welcomes steps to improve the system, but they must come with proper funding and ensure they don’t overload health-care aides or support workers.
Other recommendations include an internal waiting room surge protocol, improvements to patient oversight and communication, and larger system-wide measures to improve wait times and patient flow.
Asagwara said action has been taken on all of the 17 recommendations. The review’s findings and recommendations were shared with Giffin’s family.
“That tragedy provided opportunities for us as a system to improve and to learn, and that work continues to be done.”–Health Minister Uzoma Asagwara
His sister, Ronalee Reynolds, said her family is satisfied with the review and the steps taken by the province and Shared Health, which operates HSC.
She said her family does not place blame on front-line staff nor any fault on Shared Health. Some recommendations will require additional employees, she noted.
“I just hope that they do get the staffing. I think that is the biggest issue,” Reynolds said.
Initially, Giffin’s family had a number of questions, including what caused his death and how many times he was assessed between the time he arrived and the time he was found unresponsive.
Reynolds said a report from the Office of the Chief Medical Examiner listed her brother’s primary cause of death as acute bacterial pneumonia.
After arriving just before midnight and being triaged, he was checked in the waiting room at about 2:30 a.m. and 5 a.m., she said.
Giffin’s vital signs and breathing were good, and his oxygen levels were fine, Reynolds said.
“Everything was normal. There was no reason for them to believe he had pneumonia to begin with,” she said.
At about 7 a.m. — about an hour before staff noticed his condition had worsened — he told an employee he was fine.
“They didn’t do any checks because he was alert, and he said he was OK and he didn’t need anything,” Reynolds said.
Giffin, who had been homeless and struggled with mental health issues and addictions, was under the care of the public guardian and trustee. Paramedics took him to the ER after he was found outside in the cold by a concerned person near Main Street and Henry Avenue.
Reynolds was informed that her brother, who estranged himself from his family about a decade ago, told the public guardian and trustee he had no next of kin.
“I just hope that they do get the staffing. I think that is the biggest issue.”–Ronalee Reynolds, Chad Giffin’s sister
Giffin’s family learned about his death from a journalist. Reynolds has said a Shared Health official contacted her three days after the death to confirm Giffin was the man who had died in the ER, prompting concerns about next-of-kin notification processes.
At the family’s request, health authorities were instructed to amend policies when it comes to notifying the next of kin of patients under the care of the public guardian and trustee.
There were also questions about the communication between Shared Health and Asagwara’s department after Giffin died.
Internal emails obtained by the Globe and Mail through a freedom of information request showed deputy health minister Scott Sinclair found out about Giffin’s death hours later and after it was reported by media.
On Thursday, Asagwara said they and their office were notified of the death “not soon enough.”
“The information did not flow as quickly as it should have,” they said. “As the minister, there are a few things that are fundamentally important in terms of how our relationships with regional health authorities and leaders across the system function.”
“Accountability, transparency and communication are key, whether you’re talking about finances… or tragedies,” the minister said.
chris.kitching@freepress.mb.ca

Chris Kitching is a general assignment reporter at the Free Press. He began his newspaper career in 2001, with stops in Winnipeg, Toronto and London, England, along the way. After returning to Winnipeg, he joined the Free Press in 2021, and now covers a little bit of everything for the newspaper. Read more about Chris.
Every piece of reporting Chris produces is reviewed by an editing team before it is posted online or published in print — part of the Free Press‘s tradition, since 1872, of producing reliable independent journalism. Read more about Free Press’s history and mandate, and learn how our newsroom operates.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.







