Lost in transition From insomnia to night sweats, women aged 40-plus fight stigma — and sometimes doctors — to treat perimenopause
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$1 per week for 24 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $4.00 plus GST every four weeks. After 24 weeks, price increases to the regular rate of $19.95 plus GST every four weeks. Offer available to new and qualified returning subscribers only. Cancel any time.
Monthly Digital Subscription
$4.99/week*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*Billed as $19.95 plus GST every four weeks. Cancel any time.
To continue reading, please subscribe:
Add Free Press access to your Brandon Sun subscription for only an additional
$1 for the first 4 weeks*
*Your next subscription payment will increase by $1.00 and you will be charged $16.99 plus GST for four weeks. After four weeks, your payment will increase to $23.99 plus GST every four weeks.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 19/11/2023 (804 days ago), so information in it may no longer be current.
Usually a deep sleeper, Anne Jackson, 51, started having trouble two years ago. She would wake up throughout the night, every 90 minutes or so, and struggle to lull herself back to sleep.
Her nighttime woes escalated to the point where her doctor prescribed sleeping pills. She takes them sparingly; the pills are highly addictive.
Silenced Symptoms
Downplayed. Dismissed. Devalued.
In this monthly Free Press series, we’ll explore underdiagnosed, underrecognized and undertreated health issues affecting the lives of women, nonbinary and trans people. We will share stories and lived experiences, while also raising awareness.
In this instalment, we look at perimenopause.
“The lack of sleep really bothers me, because I am groggy and tired and not as efficient at work,” she says. “Then at 3 p.m. I get really really tired. It throws my whole system off.”
Jackson’s inability to get a good night’s rest was the first symptom of perimenopause, the transitional period that leads into menopause. Since then she’s had to navigate brain fog, weight gain, hot flashes and crippling joint pain.
She is just one of more than 10 million Canadian women aged 40-plus whose perimenopausal symptoms are often dismissed, misdiagnosed or trivialized. Many of these women are at the peak of their careers and/or raising children as they try to manage the often debilitating physiological changes.
Symptoms, of which there are more than 30, can appear as early as 10 years before menopause itself, which is defined as 12 consecutive months without a period.
The average age of menopause is 51 1/2 years, so realistically, perimenopause can begin when a woman is in her late 30s or early 40s.
MIKE DEAL / WINNIPEG FREE PRESS Dr. Omolayo Famuyide is the Medical Director and Founder of the Layo Centre and an expert in the area of women’s health.
During perimenopause — during which women will continue to menstruate, although their periods may become irregular — levels of estrogen in the body start to decrease, creating a raft of symptoms which include, but are not limited to, headaches, irregular and/or heavy periods, vaginal dryness, mood disturbances, joint pain, hair loss, memory issues and hot flashes.
There are a number of treatments and therapies on offer to manage symptoms, including prescription medication such as hormone therapy, vaginal creams and hormone-free drugs dealing specifically with hot flashes.
Eating a nutritionally balanced diet, exercising regularly, avoiding too much alcohol and practising stress-reduction techniques such as yoga or meditation are also recommended by medical professionals.
Jackson counts herself fortunate to have a doctor who not only listens, but has prescribed painkillers and massages to manage her pain.
“I have a wine group with six other women and when we talk, they tell me their men doctors just dismiss all their symptoms,” she says.
“I think I am one of the lucky ones, because I have a female doctor who is very supportive.”
Perimenopause is rarely discussed publicly. Considered a conversational taboo, the condition experienced by half the population is often also misunderstood.
“It’s interesting how many women are still quite surprised to see this is what it is,” says Dr. Omolayo Famuyide, a certified menopause practitioner, medical director and founder of the Layo Centre, formerly known as the Winnipeg Women’s Health and Contraception Clinic.
“I hear a lot of ‘I just thought I was going crazy; this is not me.’ And then when you see them after intervention, you hear things like ‘I feel like I have my life back,’” she says.
In a culture where a woman’s most valuable asset is her youth, perimenopause is stigmatized, owing to its negative association with decay and decline.
“Overwhelmingly viewed as negative, the image of a perimenopausal woman is an unflattering one, which is why many women do not want to be associated with it,” says Janet Ko, co-founder and president of the Menopause Foundation of Canada (MFC).
Ko created MFC with Trish Barbato when they started experiencing symptoms neither could explain.
Supplied Janet Ko is president and co-founder of Menopause Foundation of Canada. She says that most people’s view of perimenopause is overwhelmingly negative.
“I had never heard of perimenopause, did not know, did not understand it could last up to 10 years,” she says. “I thought menopause would be great — no periods, no pregnancy.”
Instead she suffered from heart palpitations, brain fog, joint pain, fatigue, body aches, anxiety and hot flashes.
“It’s such an injustice that there is so little awareness and knowledge. When women don’t understand what is happening to their bodies, then they are not able to proactively manage their health,” she says.
“A survey we did in 2022, The Silence and the Stigma: Menopause in Canada, revealed one in two women are unprepared for menopause. It is still a taboo topic and many women have very low levels of understanding the symptoms of peri and menopause.”
“I think there is a shift is happening, but I think a lot of women are completely perplexed,” Famuyide agrees. “Not everyone presents with the same symptoms. If we look on a global scale, research and funding regarding women’s health doesn’t get the level of investment as men’s health.
“As a society, there is a taboo speaking about female parts … You will see advertisements around erectile dysfunction on television, but you won’t hear much about perimenopause.”
The lack of knowledge, especially about the potentially early onset of perimenopause, can mean that women who choose to delay childbirth find themselves unable to conceive.
“This opens up the conversation about age,” Famuyide says. “By age 35, a majority of women will have experienced a significant decline in their fertility. Women should be having these conversations with their (health care) providers if they are concerned about the ability to conceive after 35.”
“It’s such an injustice that there is so little awareness and knowledge. When women don’t understand what is happening to their bodies, then they are not able to proactively manage their health.”–Janet Ko
In Manitoba, the closure of the Mature Women’s Centre at Victoria Hospital by the previous Progressive Conservative government meant women lost access to an expert team of multidisciplinary specialists.
During their campaign period the NDP promised to rebuild the health centre.
Health Minister Uzoma Asagwara says the NDP is committed to reopening the facility.
“It is far too early for us to set a date for the reopening, but we are actively working, meeting with experts and organizations locally, to strengthen mature women’s health care in Manitoba and move in a direction that will allow us to open the mature women’s clinic,” Asagwara said.
Access to specialist care will allow women to be more informed about the treatments available to manage symptoms.
Often Dr. Famuyide’s patients, who are referred to her by their general practitioners, have been misdiagnosed.
“Vaginal symptoms such as dryness and itchiness are often mistaken for UTIs; mood disturbances are misdiagnosed as anxiety or depression; and brain fog attributed to forgetfulness due to stress,” she explains.
“Women of colour in particular are often overlooked, as they experience menopause differently. One thing people don’t know is that Black women tend to experience menopause earlier, because they tend to present with periods earlier.”
MIKE DEAL / WINNIPEG FREE PRESS Dr. Omolayo Famuyide is the medical director and founder of the Layo Centre and an expert in the area of women’s health.
Women who experience severe PMS symptoms or post-partum depression will often experience mood disturbances during perimenopause.
“The mood disturbances can range from ‘I can’t stand my kids’ to women presenting as clinically depressed, where they are taking time off work,” Famuyide says. “A lot of these times women might get put on anti-depressants, but when you look at the time period when this starts happening, this is hands-down perimenopause and a lot of them do well on hormone therapy,” she says.
Concerns about using menopausal hormone therapy (MHT), previously referred to as hormone replacement therapy, were first raised in the 1990s, when a study found association with higher rates of breast cancer and stroke.
However, experts now say risks were overstated; women in their 40s and 50s present much lower risks, especially if they use hormone therapy for five years or less.
A paper published in the Canadian Medical Association Journal in May states that women suffering from severe symptoms should be presented with the option of hormonal therapy.
“There’s a whole constellation of menopausal and perimenopausal symptoms, some of which can be extremely debilitating, especially to what is relatively a young woman in our day and age,” says Dr. Iliana Lega, an endocrinologist at Women’s College Hospital in Toronto and the paper’s lead author.
The review paper said MHT is up to 90 per cent effective in treating hot flashes and improves sleep quality and mood disturbances. It also helps prevent the loss of bone density.
Workplaces need to become menopause-inclusive: report
Menopause Foundation of Canada’s Menopause and Work in Canada report, published in October 2023, estimates that the unmanaged symptoms of menopause costs the economy $3.5 billion per year.
Menopause Foundation of Canada’s Menopause and Work in Canada report, published in October 2023, estimates that the unmanaged symptoms of menopause costs the economy $3.5 billion per year.
Within the country’s 20 million person labour market, five million are working women ages 40-plus, two million of whom are working women between the ages of 45 and 55.
Women continue to make up the bulk of historically female-dominated sectors, such as: health care/social assistance (81 per cent) and education (69 per cent).
They are well-represented in areas like government services (65 per cent), business (64 per cent), and finance (50 per cent); other sectors increasingly rely on women too, including agriculture (30 per cent), construction (29 per cent), manufacturing (29 per cent) and mining (19 per cent).
The dominant age group in some sectors also closely matches the menopause years — 50 per cent of nurses in Canada, for example, are women over the age of 40.
The report showed that women are leaving the workforce in their prime — there is a 14 per cent drop in the number of working women in Canada between 45 (85.9 per cent work) and 59 (71.9 per cent work), compared to a 10 per cent drop for working men.
Unmanaged symptoms account for $237 million in lost productivity, 540,000 lost days of work attributed to menopause symptom management and $3.3 billion in lost income due to reduction in hours and/or pay or leaving the workforce altogether.
One-third (32 per cent) of working women say their menopause symptoms negatively impacted their performance at work while one-quarter (24 per cent) say they hid their symptoms at work. One in five women (22 per cent) believe their symptoms could affect their progression at work.
One in two women in Canada say they are unprepared for menopause with less than one-quarter of survey respondents believing they are very knowledgeable about the signs and symptoms of perimenopause and menopause.
Workplace stigma plays a role, too. The fear of being judged as past their prime can cause many women to minimize their symptoms or not share what they are experiencing.
The report identified two million women in the Canadian workforce, in their perimenopausal, menopausal and post-menopausal years, who are not being supported by their employers.
More than half of the women surveyed said they felt uncomfortable speaking to their supervisor about their symptoms.
“Lack of knowledge about menopause, challenges accessing care and stigma in the workplace impacts women’s ability to thrive in the prime of their working lives,” MFC co-founder Janet Ko says. “What we know is that women are stepping back, going part-time or taking the lesser role because they are not getting the help they need.”
Three-quarters of the women surveyed in the report said they would like to see workplaces offer supports such as flexible work arrangements, medical insurance that covers menopause treatments and therapies and educational and awareness toolkits for managers and colleagues.
“Workplaces need to become menopause-inclusive to stem the tide of women leaving,” Ko says. “First and foremost, it comes to closing the knowledge gap and breaking the stigma.”
While MHT is not recommended for everyone, benefits far outweigh the risks for those who are under 60 and are not at risk of breast cancer or blood clots, the paper states.
“MHT is therapies and medication that we use to treat women who present with moderate to severe symptoms that would classically consist of a pill, a patch or gel,” Dr. Famuyide says.
“We have many different options now. Medication is just one piece of the puzzle. You cannot change how your body will go through perimenopause, but there are preventative things you can do, like incorporating movement into your routine and eating a nutritionally balanced diet.”
The Associated Press files More women suffering “debilitating” symptoms of menopause should be presented with the option of hormonal therapy, a paper published in the CMAJ medical journal in October says.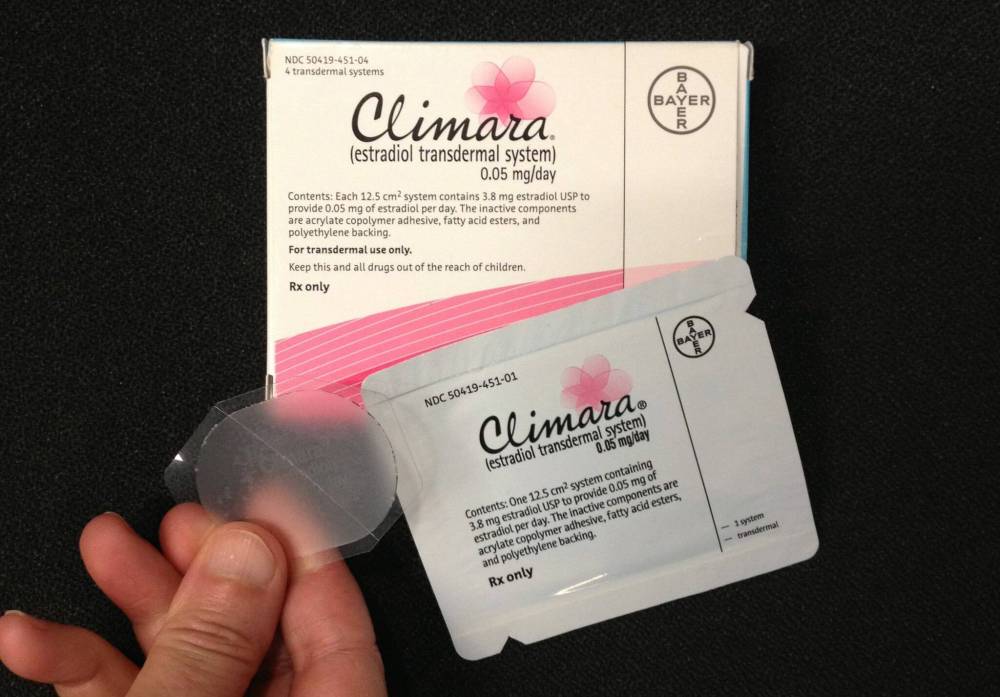
Ultimately, she says women should feel empowered to seek information. There is no need to suffer in silence.
“It is OK to not be OK. Your symptoms are valid; what you are going through is not in your head — it is an actual physiological thing that is happening.
“Just because you haven’t been diagnosed with a big cut on your leg doesn’t mean you don’t have a wound. This is significant, this is important.”
Widely fluctuating hormones during the transitional perimenopausal period are an almost universal experience and yet no one really talks about it, afraid of being told they are “making a fuss” or “exaggerating.” The culture of silence and shame is so pervasive, it was difficult to find women who were willing to share their experiences with the Free Press when we were looking for voices to feature.
One interviewee said her male friends think she’s “whining” when she complains about lack of sleep or declining stamina.
“They don’t understand it’s a real problem. I can’t do the things I was once able to do. I want to get it fixed; I want to put all of this behind me,” she said, speaking on condition of anonymity.
Jolyn Hoogstraten realized something was amiss when her jeans started to feel uncomfortable. After wearing denims for years, Hoogstraten, 52, suddenly couldn’t bear the thought of them touching her skin.
“It was a feeling (like) I needed to pee very frequently. I remember it specifically because I had to stop wearing jeans, as they made my vagina feel so uncomfortable, and I started wearing tights only,” Hoogstraten shares.
She kept visiting her doctor, as she thought she was suffering from recurrent urinary tract infections.
“They were unable to find bacteria in my urine but kept offering me antibiotics,” she says.
MIKAELA MACKENZIE / WINNIPEG FREE PRESS Jolyn Hoogstraten, 52, is vocal about her experience with perimenopause and advocates for a more open dialogue on women’s health.
Other than needing to use the toilet frequently, there was no indication she was experiencing perimenopause.
“This went on for about two years,” she says. “I was seeing a female doctor regularly who never once mentioned anything to me about possible perimenopause, vaginal menopause, hormonal changes… nothing.”
Hoogstraten figured out what was going on by chance, when she spotted a billboard advertising pelvic-floor physiotherapy. Her research into the treatment led her to a Facebook group, Menopause Chicks, where she found posts from other women experiencing the same symptoms.
The posts spurred her to book an appointment with a pelvic-floor physiotherapist, where she learned her pelvic floor had fallen and that she had Stage 2 bladder prolapse.
She started learning to use her muscles to support her pelvic floor. She also invested in an expensive hyaluronic acid vaginal moisturizer, which she used up to five times a day.
Hoogstraten was experiencing vaginal atrophy, also known as genitourinary syndrome of menopause, a condition that can occur during perimenopause when ovaries produce less estrogen. This causes the tissues of the vulva and the lining of the vagina to become drier, thinner and less elastic.
“Once I realized what was going on, I knew why it was so uncomfortable for me to sit or to wear normal pants. The mucous membranes which should have been creating lubrication on the outer and inner labia were inflamed, swollen and sticking together,” she says.
Her worst bout of vaginal dryness lasted six weeks, when she experienced a loss of control of her pelvic floor. Even her moisturizer had stopped working.
“I went into a walk-in clinic, saw a male doctor and as soon as I started describing my symptoms he put his hands up and said, ‘I can’t deal with this; I am going to refer you to a menopause specialist.’ I was losing my mind. I asked him if he could give me anything right then, as I couldn’t function. It was absolutely debilitating and all he could tell me was that I needed a blood test and I had to wait to see a specialist,” she recalls.
Hoogstraten later found out that the doctor could have immediately prescribed her a vaginal estrogen cream without her having to undergo a blood test.
“To his credit, he did send me a referral and I saw the excellent Dr. (Jennifer) Malmstrom at the Concordia Clinic. We had a thorough consultation and because I was not experiencing other symptoms, such as extreme bleeding and hot flashes, she gave me a prescription for the cream.
“I used the cream and the next day I felt completely different … now my vagina is just my vagina — it’s magical and incredible and beautiful — and I can wear jeans again,” Hoogstraten says with a laugh.
“I am one of the lucky ones who was able to access and find the information I needed. I want to see more people being educated about this … We need to take the stigma away from it.”–Jolyn Hoogstraten
Hoogstraten is vocal when it comes to sharing her experiences; she doesn’t want anyone else to go through what she went through.
“I am one of the lucky ones who was able to access and find the information I needed. I want to see more people being educated about this … We need to take the stigma away from it; it’s a bodily function that 50 per cent of the population will experience. It’s time to speak up, to say, ‘Something is wrong, let’s try to fix it.’”
It came from nowhere. Suddenly, after years of being able to rely on her stellar memory, Golda Ferrer, 44, started to forget facts. For someone who always prided herself on her remarkable recall, this state of affairs was alarming.
Then Ferrer’s periods started to become heavier. She would often have to wear overnight sanitary pads during the day, changing them every two hours. This, coupled with unusual bloating, mood changes and painful headaches, prompted Ferrer to seek medical advice.
“I always think it’s stress at first. I don’t get headaches, so when I do get them, I always worry. I am very religious about medical things when it comes to my female reproductive stuff. I am very proactive.
“I saw my gynecologist, but they did not take me seriously. They will gladly do bloodwork to check my iron levels but they refused to do any kind of hormonal check. They always switch birth control, they say the mood changes are signs of depression.”
Visits to her gynecologist are frustrating.
MIKAELA MACKENZIE / WINNIPEG FREE PRESS Golda Ferrer at the hair salon where she works. A change in her memory was one of her first signs of perimenopause.
“I am irritated when I go to my gyne. For them to pass this on to my mental health is actually them passing the buck on my reproductive health,” she says.
It was during a visit to her visceral massage therapist when Ferrer realized she might be experiencing perimenopausal symptoms.
“(My therapist) is a former nurse and she told me I was perimenopausal after a few visits. I never assumed it was perimenopause — I have gone to see my doctor about it but he didn’t refer me to a specialist. I want to see a specialist,” she says.
For now Ferrer is managing her symptoms by making changes to her lifestyle. She says she has modified her diet and has started to explore non-western therapies.
“To some extent I have accepted it but I still want to be referred to a specialist,” she says.
“If this was a disease that men had, there would be clinics devoted to it, specialists devoted to it and here we are as women having to individually research and navigate and find our way through things, because there is no central, cohesive, reliable source of information and education,” says Gwen Rowe, 49.
Rowe, who is now in menopause, says her symptoms included fallen arches, cracked heels, dry skin, thinning hair, acid reflux and irritability.
She’s still dealing with brain fog and insomnia.
The Brandon-based reflexologist says that having to navigate perimenopause by herself made her passionate about sharing her experience with others.
“Women want information; they don’t want to feel alone. Most of the women coming to see me are all going through the same thing. We are smart, we are educated and we have had enough; it’s time we had supports from the medical system, our work system and, quite frankly, each other.
“We have to stop feeling embarrassed to talk about it.”
av.kitching@freepress.mb.ca

AV Kitching is an arts and life writer at the Free Press. She has been a journalist for more than two decades and has worked across three continents writing about people, travel, food, and fashion. Read more about AV.
Every piece of reporting AV produces is reviewed by an editing team before it is posted online or published in print — part of the Free Press‘s tradition, since 1872, of producing reliable independent journalism. Read more about Free Press’s history and mandate, and learn how our newsroom operates.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.
History
Updated on Sunday, November 19, 2023 4:05 PM CST: Minor formatting
Updated on Monday, November 20, 2023 7:34 AM CST: Adds photo
Updated on Monday, November 20, 2023 1:00 PM CST: Removes duplicate excerpt


